In Australia we are in the throes of a severe cold and flu season. As well as the usual viral suspects such as influenza, RSV and rhinovirus (which causes the common cold), bacterial pathogens are also causing significant rates of illness, particularly in children. These include: Bordetella pertussis (whooping cough) and Mycoplasma pneumoniae,
Meanwhile, SARS-CoV-2 (the virus that causes Covid) is responsible for recurring waves of infections as it evolves and mutates into new forms that keep it one step ahead of our immunity.
The latest variant is named “FLuQE”, and is reportedly gaining popularity in Australia and other countries. So what is worth knowing about FLuQE?
From FLiRT to FLuQE
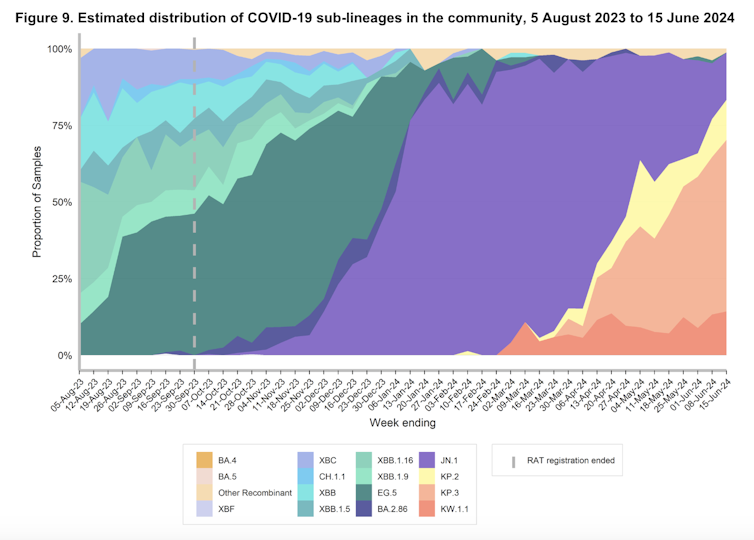
In recent months, you may have heard of the “FLiRT” subvariants. These are descendants of the Omicron variant JN.1, including KP.1.1, KP.2, and JN.1.7.
KP.2 contributed significantly to Covid infections in Australia and elsewhere, particularly around May.
The name FLiRT refers to amino acid substitutions in the spike protein (F456L, V1104L and R346T). Amino acids are the molecular building blocks of proteins, and the spike protein is the protein on the surface of SARS-CoV-2 that allows it to attach to our cells. These changes in the spike protein arise from mutations – random changes in the genetic code of the virus.
The goal of SARS-CoV-2 is to select mutations that produce a spike protein that supports efficient infection (sometimes called viral fitness) by binding strongly to receptors on our cells, while also evading neutralizing antibodies in our immune system (immune pressure).
The FLiRT mutations reduce the ability of neutralising antibodies to attach to the spike protein, helping the virus to evade our immunity. But at the same time, it appears that the immune pressure that selected for these mutations has affected the virus’ ability to attach to our cells.
These findings have yet to be peer-reviewed (independently verified by other researchers). However, they suggest that the FLiRT variant has swapped some of its ability to infect our cells for a spike protein that is more resistant to our immune system.

According to experts in Australia and internationally, what has happened with FLuQE is that an additional mutation has restored fitness that was lost with the FLiRT mutation.
FLuQE (KP.3) is a direct descendant of FLiRT, meaning it inherited the same mutations as the FLiRT variant. But it has an additional amino acid change in the spike protein, Q493E (giving FLuQE its name).
This means that the amino acid glutamine at the 493rd position has changed to glutamic acid (the spike protein is 1,273 amino acids long). Glutamine is a neutral amino acid, while glutamic acid has a negative charge, which changes the properties of the spike protein. This may improve the virus’s ability to infect our cells.
It’s still early days for FLuQE and we don’t have peer-reviewed research on it yet. But it seems we now have (another) immune-evading virus that is also well-adapted to infecting our cells. So, it’s no surprise that FLuQE is becoming prominent in many countries.
what next?
We expect that with widespread transmission and infection of the FLiRT and FLuQE variants, population immunity to these variants will mature, and over time, their dominance will be replaced by the next immune-evading variants.
The tug of war between our immune system and SARS-CoV-2 evolution continues. The issue we are dealing with now is that vaccines do not adequately protect against infection or suppress transmission of the virus. While they are very good at preventing severe disease, the virus still infects many people.
As well as putting a strain on people and the health service, lots of infections mean more opportunities for the virus to evolve. The more “dice” the virus has to find mutations that help it evade our immune system and infect our cells, the more likely it is to do so.
Next-generation vaccines and treatments really need to boost immunity in the upper respiratory tract (nose and throat) to reduce infection and transmission. This is where infection starts. A human challenge study, where volunteers were experimentally exposed to SARS-CoV-2, showed that those who did not become infected had a strong anti-viral immune response in the upper respiratory tract.
To this end, there are immune-stimulating nasal sprays and nasal vaccines in clinical development. The hope is that this approach will slow the evolution of SARS-CoV-2 and the emergence of new subtypes that continue to drive waves of infection and disease.
Fortunately, so far these mutations have not resulted in a virus that is clearly more pathogenic (causing more dangerous disease), but there is no guarantee that this will not happen in the future.![]()
,Author: Nathan Bartlett, Professor, School of Biomedical Sciences and Pharmacy, Newcastle University)
,disclosure statement: Nathan Bartlett does not work for, consult, hold shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond his academic appointment)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
(Except for the headline, this story has not been edited by NDTV staff and is published from a syndicated feed.)